Telehealth, the practice of delivering healthcare services remotely through digital platforms, has grown tremendously in recent years. This technology-driven approach has opened new doors for both patients and healthcare providers, allowing greater access to care, especially in underserved areas. Telehealth saw a significant surge during the COVID-19 pandemic, it remains a vital option in modern medicine and one of the handful of places nurses can work. However, while telehealth offers a number of benefits, it also comes with some challenges. In this article, we’ll explore the pros and cons of telehealth, providing a balanced perspective on its impact on healthcare delivery.
 Pros of Telehealth
Pros of Telehealth
1. Improved Access to HealthCare
One of the most significant advantages of telehealth is that it improves access to medical care, particularly for individuals in rural or underserved areas. For many people living in remote regions, getting to a healthcare facility can involve long travel times and significant costs. Telehealth eliminates these barriers by enabling patients to consult with healthcare providers from the comfort of their own homes.
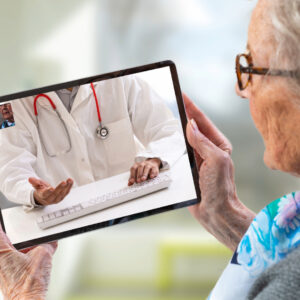
This expanded access is also beneficial for individuals with mobility issues, the elderly, or those with chronic conditions that make traveling to a doctor’s office challenging. Telehealth allows these patients to receive timely care without the added burden of physically getting to a clinic or hospital.
2. Convenience and Time Savings
Telehealth appointments save time for both patients and healthcare providers. Rather than sitting in a waiting room or spending hours commuting to and from appointments, patients can log into a video call from their home, office, or even while traveling. This convenience is especially valuable for busy individuals who may find it difficult to take time off work or arrange for childcare.
For providers, telehealth can streamline workflows and reduce administrative burdens. Doctors can see more patients in less time, and the reduced need for in-person visits can help healthcare facilities manage patient volumes more effectively.
3. Reduced Risk of Infections
Telehealth also minimizes the risk of exposure to infectious diseases, both for patients and workers. In traditional clinical settings, patients waiting for care are often in close proximity to others who may have contagious illnesses. For people with weakened immune systems or chronic conditions, avoiding such exposure is critical.
During the COVID-19 pandemic, telehealth played a vital role in reducing the spread of the virus by allowing people to consult with doctors without the need for in-person visits. This benefit extends beyond pandemic scenarios, as telehealth can help reduce the transmission of common infectious diseases like the flu.
4. Improved Patient Engagement and Follow-Up
Telehealth can improve patient engagement by making it easier for individuals to follow up with their healthcare providers. For many people, traditional in-person follow-up appointments can feel burdensome, leading to missed visits and gaps in care. With telehealth, scheduling follow-up appointments is more flexible, making it easier for patients to stay connected with their doctors and adhere to treatment plans.
In addition, telehealth can facilitate more frequent communication between patients and providers, improving health outcomes. For instance, patients managing chronic conditions like diabetes or hypertension can have regular virtual check-ins with their doctors to monitor progress and make necessary adjustments to their care plans.
5. Cost Savings
Telehealth can lead to cost savings for both patients and providers. Patients save money on travel expenses, and in many cases, telehealth visits are less expensive than traditional in-person consultations. For healthcare facilities, telehealth can reduce overhead costs associated with running a physical clinic, such as utilities, administrative staffing, and building maintenance.
Additionally, telehealth can help reduce the number of unnecessary emergency room visits by providing patients with timely access to care. This not only saves patients money but also helps alleviate the burden on overcrowded emergency departments.
Cons of Telehealth
1. Limited Physical Examinations
One of the primary drawbacks of telehealth is that it limits the ability of providers to conduct thorough physical examinations. While video calls allow for visual assessments, certain aspects of a physical exam—such as checking vital signs, palpating areas of pain, or listening to a patient’s heart and lungs—cannot be replicated remotely.
This limitation means that telehealth may not be suitable for all medical concerns. Conditions that require in-depth physical examinations or diagnostic tests may still necessitate an in-person visit, which can reduce the overall convenience of telehealth for certain patients.
2. Technological Barriers
Telehealth relies on access to technology, such as smartphones, computers, and high-speed internet. For some patients, particularly older adults or those in low-income areas, these technological requirements can pose significant barriers. Not everyone has the necessary equipment or digital literacy to successfully participate in telehealth consultations.
In addition, technical issues such as poor internet connectivity, software glitches, or unfamiliarity with video conferencing platforms can disrupt telehealth appointments, leading to frustration for both patients and providers.
3. Privacy and Security Concerns
The rise of telehealth has also raised concerns about patient privacy and data security. Healthcare providers are required to comply with regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S., which ensures that patient information is protected. However, telehealth platforms may still be vulnerable to cyberattacks or data breaches.
While reputable telehealth providers use encrypted communication systems to safeguard patient data, there is always a risk when transmitting sensitive health information over the internet. Patients must trust that their telehealth provider is using secure, compliant systems to protect their privacy.
4. Reduced Personal Connection
Some patients and providers express concerns about the reduced personal connection in telehealth consultations. In-person interactions often help build trust and rapport between a doctor and patient, which can be more difficult to achieve over a video call. Body language, eye contact, and other non-verbal cues can be harder to read in virtual settings, potentially affecting the quality of communication.
For some patients, especially those with complex medical conditions or mental health concerns, the lack of face-to-face interaction can feel impersonal and less supportive. This reduced connection may impact patient satisfaction and the overall quality of care.
5. Insurance and Reimbursement Issues
While telehealth is increasingly recognized as a viable method of delivering care, insurance coverage for telehealth services can vary depending on the provider, state regulations, and healthcare plan. Some insurers may not cover telehealth appointments to the same extent as in-person visits, leaving patients with out-of-pocket costs.
Additionally, reimbursement rates for telehealth services may be lower for providers, which can discourage widespread adoption of telehealth in some practices. These financial barriers need to be addressed to ensure telehealth is accessible and sustainable for both patients and providers.
Conclusion
Telehealth has brought significant benefits to the healthcare industry, offering increased access, convenience, and cost savings for many patients and providers. It has proven to be particularly valuable in remote areas and during public health crises, such as the COVID-19 pandemic. However, telehealth also comes with limitations, such as reduced physical examinations, technological barriers, and potential privacy concerns. While telehealth is unlikely to replace in-person care entirely, it offers a valuable complement to traditional services.
As technology continues to advance, and as healthcare systems adapt to new models of care delivery, telehealth will likely become an even more integral part of the way things work. By addressing its challenges and maximizing its strengths, telehealth can play a key role in improving health outcomes and making healthcare more accessible and patient-centered in the future.


